 Dr Penny Fraser MB BS BSc(HONS) MRCS(ENG)
Dr Penny Fraser MB BS BSc(HONS) MRCS(ENG)
Dr Penny is a British-trained Emergency Medicine doctor, who lives in Geneva. She is also the mother of two girls aged 9 and 10. Along with Dr Michelle Wright and her other colleagues at HealthFirst, she has a passion for delivering health education and First Aid training to the English-speaking community in Switzerland.
HealthFirst provides a range of practical, interactive First Aid courses including a unique Mountain First Aid Course and a First Aid course, obligatory for the Swiss Driver’s Licence, and suitable for anyone from the age of 14.

For this blog, I have invited HealthFirst’s Midwife and mother of four, Polly Pupulin, to give us her 5 top tips for expectant mothers....
By Polly Pupulin, Midwife, www.healthfirst.ch
I love midwifery and have done since I first started in 2001. Part of my work is the privilege to introduce parents to the amazing ‘dance’ that happens between the baby and mother during pregnancy and labour during a Birth Preparation Course.
If I could personally give five tips to every expectant parent here in Switzerland, this is what I would say:
1. You have a choice where and how you birth your baby. The birth is not just a medical procedure but involves many other factors such as your personal preferences, your cultural expectations, your previous experiences of childbirth and what both you and your partner believe birth is all about.
2. The best form of ‘natural’ pain relief is a supportive birth partner and a compassionate midwife in whom you have confidence. You may have heard of epidurals – and they definitely have their place – but there are many compatible and harmonising pain relief options to learn about.
3. The labour process is a blend of you and your baby working together. Both of you have a role and will be communicating together. Knowing this may calm you and help you feel part of a loving team.
4. Yes, your life will change when your baby is born. However everyone reacts and adjusts differently and you won’t know until the challenge is there. So welcome to the journey – and enjoy it!
5. You may be away from your normal family support network in your home country but you are not alone. Create or join a new group of like-minded parents and parents-to-be here in your country of residence – in person and online. Having this support within your own community is proven to reduce your risk of post-natal depression.

Mild head injuries are common, especially in children and during contact sports. They can occur when the head is hit by a moving object (e.g. a ball, car or fist) or when the head hits a stationary surface at speed (e.g. the ground, a wall etc.)
The brain ‘floats’ within the bony skull in some liquid called cerebrospinal fluid. This liquid allows a small degree of movement of the brain. If the skull is hit, then the brain may bounce or twist inside the skull. This can lead to a disruption in the electrical activity in some of the brain cells, causing them to malfunction for a short while. It is this malfunction that causes the symptoms of concussion.
The symptoms of concussion can include:
- A brief loss of consciousness at the time of the injury (followed by a rapid, spontaneous recovery)
- A loss of memory of the accident itself or the few moments before the accident happened (amnesia)
- Feeling dizzy
- Nausea
- Mild headache
These symptoms will, by definition, resolve within hours to days in most cases but may sometimes last for weeks in a few. Once all the symptoms have settled down, then a certain diagnosis of concussion can be made. There is no permanent damage to the structure of the brain when someone has concussion.

“…my hands were going pump, pump, pump. It was so basic in a way – no fancy beeping machines, hospital bed or team of medical doctors in white coats. Just the wet ground, me in my old jeans and some bystanders with a phone.”
Dr Penny Fraser, medical doctor and founder of HealthFirst, talks to her:
So, what happened that damp evening in December?
“I was on the way to pick up my six-year old daughter from her school friend’s party, when I turned a sharp bend in the road and saw a man lying in a hedge. Then I saw his bicycle lying nearby and two people standing looking at him. This looked a bit worrying to me and I thought my skills as a nurse and First Aid Trainer might be useful. So I pulled over and parked safely a little way ahead.”
What did you do next?
“I grabbed my phone and car keys then approached cautiously wondering what I might find. I asked the two bystanders what had happened and whether I could help. They both looked rather blank, shocked really, and told me that they had no idea what had happened. It was a bit wet on the ground but I just pushed into the hedge where he lay and spoke to him. He didn’t reply and when I rubbed hard on his collarbones, he just lay there unresponsive. I think he was about 60 years old and he looked very pale – white-ish or grey but the evening light was fading and it was difficult to tell.”

(c) copyright HealthFirst 2015
By Dr Penny Fraser, HealthFirst
“Coughs and Sneezes Spread Diseases”, Ministry of Health, Great Britain 1942:
What you need to know about the flu.
As the mornings are getting mistier and the kids start swapping coughs and colds at school, our thoughts may already be turning to the winter flu season – and how to avoid it.
We use the word ‘flu’ quite freely when someone has ‘just’ a cough, bad cold or fever but actually true influenza, an infection with the influenza virus A, B or C is quite a different affliction. Influenza, the ‘flu’, la grippe, die Grippe, Spanish fever – whatever you call it in your home, it is an illness that needs to be taken seriously.
It is said that the way you can tell the difference between a common cold or influenza is this: You are looking out of the window from your sick bed and see a 100CHF note lying on the grass. If you have true influenza, you just can’t get out of bed to get it!
(c) copyright HealthFirst 2015
By Dr Penny Fraser, HealthFirst
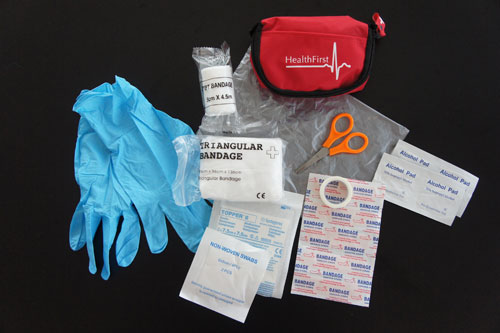
Summer is here! The school bags will soon be slung into a cupboard and the suitcases brought out to pack for holidays and family visits. Whether you are travelling by car, train or plane, the one thing that should always be taken is your First Aid Kit.
How to make an arm sling
One of the essential items that you should find in your kit is an arm-sling, used for injured collarbones, shoulders, elbows, arms, wrists and hands. Do you know why you would use one of these?
Four reasons for putting an arm sling on an injured person:
- It's a pain-killer. Every time damaged skin, muscle, tendons, bones and joints are moved, they send strong pain messages along the nerves to the brain. Ouch! If these damaged tissues are kept still and supported in an arm sling then the person will be in less pain.
- It prevents secondary injury. If the damaged tissues are kept still in the sling, then this reduces the chance of bone fragments, torn veins and ligaments wobbling about and causing worse bleeding or swelling etc.
- It accelerates recovery. It is scientifically proven that if, after an injury, people have their pain controlled and psychological stress reduced, they heal quicker. Excellent First Aid includes reassuring the person with words, gestures and eye-contact whilst putting on an arm sling.
- It gives a clear signal to others. When another person sees the arm sling, they know that the wearer is injured and needs to be cared for. A paramedic, nurse or doctor will also be able to direct their questions and treatment quickly to the injured arm, indicated by the presence of the arm sling.









